A new book by the Head of Neurosurgery offers a fresh perspective about medicine and a riveting look into neurosurgical operating rooms.
Since his first day of medical school, Dr. Christopher Honey, the head of neurosurgery at UBC, was taught that emotions impede the best practice of surgery and that he should avoid being emotionally engaged with patients. But Honey's close encounters with several patients in his 25 years as a surgeon have expanded his understanding of medicine — and what it means to be human.
“When I began surgery, I always felt that my interaction with the patient was a competition between me and the tumor,” said Honey. “And [it] took me a while, particularly as a surgeon, to learn that what I'm really doing is treating the person by attacking the illness.”
In his new book, The Tenth Nerve, Honey recounted his interactions with seven patients who fundamentally changed his perception of medicine, making him a better surgeon and person.
Innovative thinking
The name of his new book comes from his medical discovery of hemi-laryngopharyngeal spasm (HELPS) syndrome and his personal journey to discovering his relationship with patients.
The tenth nerve, also called the vagus nerve, is the longest and most complex of the 12 pairs of cranial nerves. It wanders from the brain all the way down the spinal cord into organs in the neck, chest and abdomen.
At UBC, Honey and his team discovered two diseases related to the tenth nerve that are likely to have existed since ancient times.
They discovered that a pinched tenth nerve can trigger throat contractions and coughing as the nerve controls muscles to the voicebox and sensation in the lungs. When patients were presenting with intermittent spasms of their throat, causing them to choke and pass out, nobody recognized their symptoms, because it had never been described before.
“The knee-jerk reaction in the medical field is — 'I don't understand your symptoms, you must be making this up, it's all in your head,'” said Honey. This led to his patients being misdiagnosed with a psychiatric illness and dismissed.
But one patient, Emily, was strong in her conviction that she had a physical problem. “Her courage and tenacity were an inspiration to me," wrote Honey in his new book. "She forced me to look beyond my medical training and consider the possibility of a completely new disease.”
Honey eventually decided to operate on Emily. When the pinched tenth nerve was exposed in front of his eyes, he paused and stared at it, "shocked" at the scene before him. Honey then completed the surgery and Emily’s determination finally paid off — her symptoms were resolved.
That was the first patient in the world cured of HELPS syndrome. It wouldn’t have been discovered if patients like Emily hadn’t “fought the medical system to be understood and recognized,” according to Honey. He details the unique stories of six other patients in his book.
“They taught me more about medicine than I had learned in med school,” said Honey.
Science and art
Honey’s expertise extends beyond his discovery of HELPS syndrome. His role as a neurosurgeon also includes utilizing Deep Brain Stimulation (DBS), a standard of care now for Parkinson's disease.
DBS uses electricity to modulate the brain. Through an electrode implanted in the brain’s deep structures, DBS can help ease the uncontrollable tremors characteristic of Parkinson’s disease and improve patients’ ability to move.
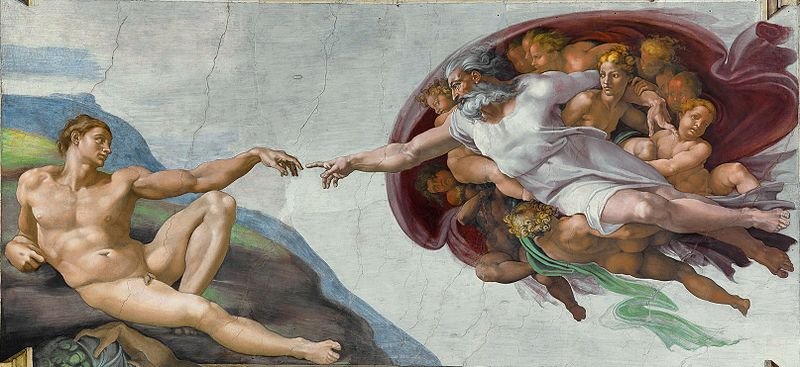
In his book, Honey detailed a touching moment between himself and a patient. During a brain surgery, Honey switched on the stimulator and, in a few seconds, watched as his patient’s tremor melted away. He held up a finger and asked the patient to touch it. The patient reached up and touched his fingertip with a steady hand, and burst into tears — that was the first time in 40 years that his tremor had ceased.
The patient later sent Honey a picture of The Creation of Adam to express how he felt at that moment. The painting depicts the Biblical creation narrative where God reaches out to touch Adam's fingertip and spark life into him.
“The ultimate goal of [DBS surgery] is to improve the patients’ quality of life,” said Honey. To accomplish this goal requires a balance between science and art, he explained.
The science part is putting the electrode in exactly the right place without hurting the patient and the demand from the surgical point of view is to put the electrode within two millimeters of the target.
But far more demanding than that, according to Honey, is the art embedded in the practice. This involves selecting the right patient — someone who will benefit from the surgery — while often balancing barriers in communication and interpersonal interaction.
“The patient is a human [who] is trying to tell you what's wrong using their language or maybe even through their children who are translating for us. And you need to understand … what is interfering with that patient's quality of life,” said Honey. “That is not mathematics, that is understanding human nature … And so I think that's an art.”
New discoveries
Honey and his team now are doing research at UBC that "no one else in the world is doing." One of the diseases that they are trying to help is a vocal disorder called spasmodic dysphonia. It causes muscles of the voice box to involuntarily squeeze tight, making it hard for patients to speak.
Honey’s team has completed the first prospective randomized trial in the world for the use of DBS to treat spasmodic dysphonia, as detailed in a study published last year in Neurosurgery.
“I think the technology of [DBS] is going to continue to help patients in British Columbia,” said Honey.“I think the indication for [DBS] will widen.”
Though DBS is currently mainly indicated in Parkinson’s disease and other movement disorders, Honey explained that the future of this procedure may have applications in epilepsy, as well mental illnesses like depression and addiction.
“We try our best to pull people back from diseases,” said Honey. He quoted Sir William Oster on the topic of the value of his patient interactions: “The good physician treats the illness, and the great physician treats the patient who has the illness,” he said.